When it comes to buying diamonds, one must tread with caution to ensure a purchase that is both valuable and authentic. In this pursuit, the Gemological Institute of America (GIA) stands as an unparalleled authority, providing a comprehensive evaluation system known as the 4Cs of Diamond Quality. This article will delve into what GIA represents and explore the advantages and benefits of understanding the 4Cs. By equipping yourself with this knowledge, you can confidently navigate the diamond market, ensuring a secure and satisfying purchase.
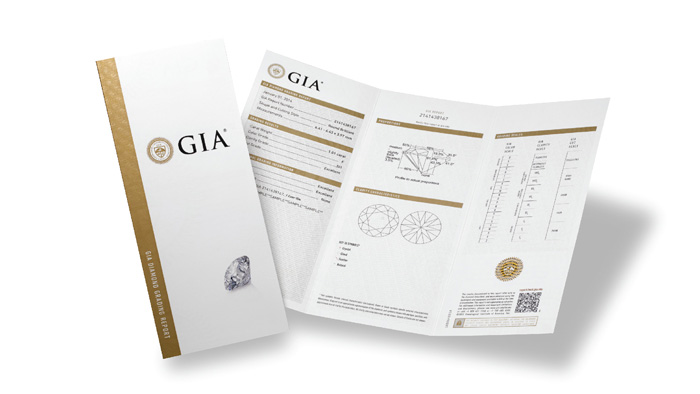
GIA: The Standard of Diamond Certification
The Gemological Institute of America (GIA) is an internationally recognized non-profit organization that has been at the forefront of gemological research and education since its establishment in 1931. With an impeccable reputation, GIA has become the global standard for diamond grading and certification. Their commitment to accuracy, integrity, and education ensures that consumers can trust the information provided by GIA reports.
The 4Cs of Diamond Quality
The 4Cs refer to the universally accepted standards for evaluating the quality and value of a diamond. Each “C” represents a specific characteristic that directly impacts a diamond’s appearance and price. Let’s explore each of these 4Cs in detail:
Cut:
The cut of a diamond refers to the precision with which it has been shaped and faceted. GIA evaluates a diamond’s cut based on its proportions, symmetry, and polish. A well-cut diamond maximizes its inherent brilliance, fire, and scintillation. By understanding the cut grade, buyers can select diamonds that exhibit optimal light performance, resulting in breathtaking sparkle.
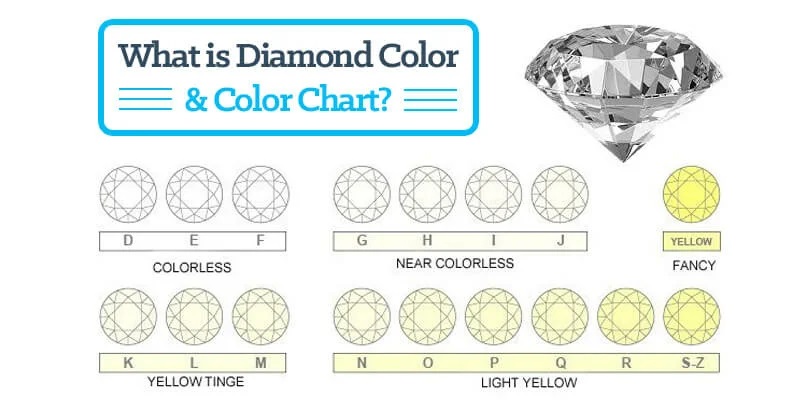
Color:
Diamonds come in a range of colors, and GIA grades them on a scale from D (colorless) to Z (light yellow or brown). GIA’s color grading system ensures consistency and accuracy across the industry. By selecting a diamond with a higher color grade, buyers can acquire stones that exhibit exceptional whiteness and brightness.
Clarity:
Clarity refers to the presence of internal and external characteristics, known as inclusions and blemishes, respectively. GIA examines diamonds under 10x magnification to determine their clarity grade. Diamonds with higher clarity grades have fewer inclusions or blemishes, resulting in exceptional transparency and brilliance.
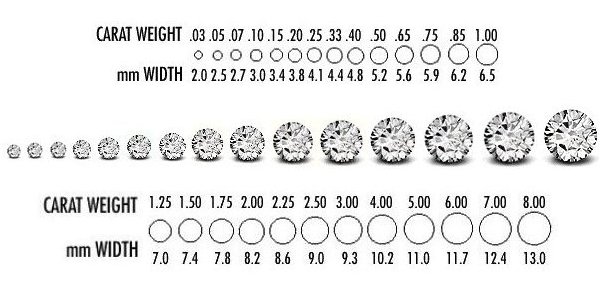
Carat Weight:
Carat weight measures a diamond’s size and is often associated with its value. GIA uses precise scales to measure and report a diamond’s weight. While carat weight is important, it is crucial to consider the other three Cs as well. By understanding how carat weight influences price and appearance, buyers can strike a balance between size and quality.
Benefits of the 4Cs
Accurate and Reliable Information:
GIA’s rigorous grading standards ensure that consumers receive accurate and reliable information about the diamonds they intend to purchase. With a GIA certificate, buyers gain confidence, knowing that they have access to a detailed analysis of their chosen diamond’s quality.
Informed Decision-Making:
Understanding the 4Cs empowers buyers to make informed decisions. By considering the interplay between cut, color, clarity, and carat weight, consumers can select diamonds that align with their preferences and budget, thereby avoiding unnecessary expenses or disappointments.
Quality Assurance:
GIA’s commitment to integrity and expertise provides an assurance of diamond quality. With a GIA certificate, buyers can trust that they are purchasing diamonds that have been objectively evaluated and graded by industry professionals.
Resale and Insurance:
GIA-certified diamonds have better resale value due to their recognized grading standards. Additionally, insurance companies often require GIA certificates for coverage, as they rely on GIA’s expertise to assess diamond quality accurately.
Expertise and Industry Standard:
GIA’s reputation as a leading authority in the diamond industry ensures that their grading and certification processes are held to the highest standards. By relying on GIA’s expertise, buyers can trust that their diamonds have been evaluated by highly trained gemologists using state-of-the-art equipment. This expertise not only provides confidence in the quality of the diamond but also adds value to the overall purchasing experience.
Consumer Protection:
GIA certification serves as a form of consumer protection, particularly in the context of online diamond purchases. With the rise of e-commerce, it can be challenging to determine the true quality of a diamond without physically examining it. However, GIA certification provides an objective and reliable assessment of a diamond’s quality, giving buyers peace of mind and ensuring that they receive what they pay for.
Timeless Value:
Diamonds certified by GIA possess timeless value. GIA’s strict grading standards ensure that the quality of the diamond is accurately reflected in the certification, establishing a lasting record of its characteristics. As a result, GIA-certified diamonds retain their value over time and can be cherished as heirlooms or passed down through generations, creating a lasting legacy.
International Recognition:
GIA’s reputation extends beyond national boundaries. Their certificates are globally recognized and respected, making GIA-certified diamonds highly sought after worldwide. This international recognition not only adds value to the diamond but also increases its desirability in the global market.
Education and Transparency:
GIA places a strong emphasis on education and transparency. Their reports provide detailed information about the diamond’s characteristics, including any imperfections or enhancements. This transparency allows buyers to make informed decisions and understand the unique qualities of the diamond they are purchasing, fostering a sense of trust and confidence in the transaction.
Ethical Sourcing and Sustainability:
GIA’s commitment to ethical sourcing and sustainability is another key advantage for diamond buyers. GIA ensures that the diamonds they certify have been responsibly sourced, adhering to strict guidelines that promote fair labor practices and environmental stewardship. By choosing GIA-certified diamonds, buyers can be confident that their purchase aligns with their ethical values and supports responsible mining practices.
Enhanced Trust and Confidence:
The 4Cs of Diamond Quality by GIA instill trust and confidence in the diamond-buying process. GIA’s independent and unbiased grading system ensures that buyers receive an accurate assessment of a diamond’s quality, eliminating doubts and uncertainties. This trust translates into a more satisfying purchasing experience, knowing that the diamond’s value is based on objective criteria established by industry experts.
Conclusion
When it comes to purchasing diamonds, GIA and the 4Cs of Diamond Quality provide a reliable framework for evaluating and selecting the perfect gem. By understanding the significance of the cut, color, clarity, and carat weight, buyers can make confident, informed decisions. GIA’s expertise, integrity, and commitment to accuracy make their certificates highly valuable in the diamond market. By prioritizing the 4Cs and seeking GIA certification, consumers can navigate the world of diamonds with ease, ensuring a secure and rewarding purchase.…